Introduction
Breast cancer is the most common cancer among women worldwide, accounting for about 1 in 4 cancer cases diagnosed in women and is one of the leading causes of cancer-related deaths in women globally. However, mortality rates have been decreasing in many developed countries due to advances in early detection and treatment.
Breast cancer is characterized by its diverse molecular subtypes, creating a heterogeneous nature of the disease. Tailoring treatment approaches based on individual characteristics becomes crucial to enhance patient outcomes.
Analysing Molecular Subtypes via Imaging
Research on radiogenomics has shown distinct imaging features associated with different molecular subtypes of breast cancer. On dynamic contrast-enhanced MRI scans, for example, oestrogen receptor-positive (ER+) tumours usually show well delineated borders and decreased enhancement dynamics, while human epidermal growth factor receptor 2-positive (HER2+) tumours usually show variable enhancement patterns. This understanding of imaging characteristics can help guide treatment planning and enable the non-invasive classification of genetic subtypes.
Predicting Treatment Response
Radiogenomic analysis is a potential approach in evaluating tumour aggressiveness and response to therapy in breast cancer patients. By comparing imaging characteristics with genetic fingerprints. Researchers can identify radiomic biomarkers associated with HER2 amplification, hormone receptor status, and chemotherapy response. Thus, with the use of this information, Clinicians can evaluate the effectiveness of therapy over time and personalise treatment plans.
Predictive Potential of Imaging Biomarkers
Radiogenomic studies have identified imaging biomarkers with prognostic significance in breast cancer, offering valuable novel insights about patient outcomes. For instance, specific texture characteristics identified from mammography or MRI images have been linked to tumor grade, lymph node status, and the risk of distant metastasis. Utilizing these imaging biomarkers in prognostic models has the potential to enhance risk assessment and guide follow-up approaches for patients undergoing treatments.
Radiogenomic Risk Prediction Models
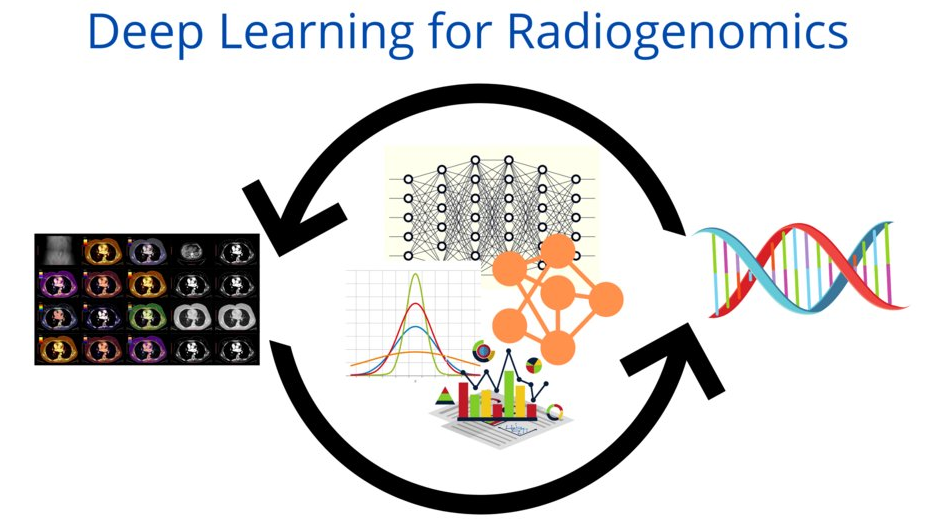
Incorporating both imaging and genomic data into holistic risk prediction models has the capacity to advance breast cancer risk stratification and clinical decision-making. Machine learning algorithms trained on multi-parametric imaging data and genomic profiles can accurately forecast patient outcomes, such as recurrence risk, survival probability, and treatment response. These models facilitate customised treatment planning and allow for individualised risk assessment in the patients with breast cancer.
Future Prospects and Clinical significance
The integration of radiogenomic analysis into routine clinical practice has the potential to revolutionize breast cancer management. Through the combined use of imaging and genomic information, healthcare providers can embrace a precision medicine strategy, tailoring treatments according to specific tumor attributes and patient needs. Moreover, ongoing advancements in radiogenomics research aim to enhance predictive models, validate imaging markers, and deepen our understanding of the biological processes influencing breast cancer advancement.
Radiogenomics offers a promising path toward deepening our comprehension of breast cancer biology and enhancing patient care. By connecting imaging with genomics, radiogenomic analysis provides valuable insights into tumor features, treatment efficacy, and patient prognoses. As advancements in this area progress, radiogenomic approaches hold the potential to revolutionize breast cancer management, enabling the development of tailored and efficient therapeutic interventions for patients.
(Author is a Radiodiagnosis student at Government Medical College, Anantnag and a researcher in precision oncology. Feedback: [email protected])