HEALTH WATCH
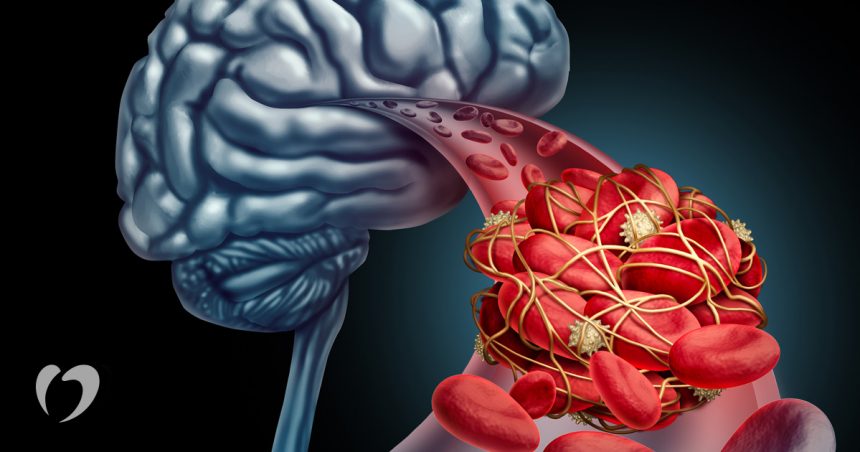
A transient ischemic attack, or TIA, is often described as a mini-stroke. Unlike a stroke, however, the symptoms can disappear within a few minutes. TIAs and strokes are both caused by a disruption of the blood flow to the brain. In TIAs and most strokes, this disruption is caused by a blood clot blocking one of the blood vessels leading to the brain. The blockage produces symptoms such as sudden weakness or numbness on one side of the body, sudden dimming or loss of vision, and difficulty speaking or understanding speech. If the symptoms are caused by a TIA, they last less than 24 hours and do not cause brain damage.
Stroke-associated symptoms, on the other hand, do not go away and may cause brain damage or death. TIAs can serve as an early warning sign of stroke and require immediate medical attention. About 85% of strokes are classified as ischemic. In ischemic stroke, a blood vessel leading to the brain becomes blocked and an area of the brain is deprived of oxygenated blood. (The other 15% of strokes are caused by bleeding from a blood vessel that has ruptured.) Without the blood supply, the cells in that area of the brain die. Since brain cells cannot grow back, the functions that are controlled by that brain area may be permanently lost.
Approximately 10% of strokes are preceded by one or more TIAs. The estimated annual number of TIAs is about 50,000; an exact count is difficult because TIAs are not always reported. They may be under-reported because they typically last less than an hour, perhaps only for a few minutes. Because they are so brief, TIAs may not seem important. However, an estimated one- third of all TIAs are followed by a stroke within five years. They are considered a medical emergency and prompt medical attention is very important.
Risk factors for strokes and TIAs are very similar. The risk of a TIA or stroke is higher among men, African Americans, people over age 65, and people with heart disease or diabetes. Smokers, people with high blood pressure, and people who are overweight also have a greater risk for TIAs and strokes.
Causes and symptoms
A TIA is caused by a temporary blockage of one of the arteries that leads into the brain. Small blood clots, called microemboli, are the immediate cause of the blockage. The blockage forms because of damage or disease within the circulatory system. Blood clots can form in blood vessels because of artery damage, heart disease, and other cardiovascular problems. For example, atherosclerosis is strongly associated with TIAs. Atherosclerosis is the build-up of fatty deposits or plaque at certain areas in the circulatory system. Clot- ting cells in blood, called platelets, tend to stick to atherosclerotic plaques or other damaged sites within blood vessels. Occasionally, a clot may grow large enough to block a blood vessel, or a piece of a clot may break off and circulate to other areas of the body. If a clot does not dissolve quickly enough, it can lodge in a blood vessel and block it. In TIAs, the microemboli dissolve within a short time.
Blood flows into the brain through two main path- ways: the carotid arteries and the vertebrobasilar arteries. The carotid arteries are located on the front of the neck; the vertebrobasilar arteries are at the base of the skull at the back of the head. The symptoms produced by a TIA are determined by the arteries affected.
If a vertebrobasilar artery is blocked, common symptoms include double vision and dizziness, nausea and vomiting, difficulty speaking, and problems under- standing and using spoken words. There may also be a numbness around the mouth and a tingling sensation in the limbs. Blockage of a carotid artery produces complete loss of vision, dimmed or foggy vision, and paralysis or weakness on one side of the body. These symptoms may also be accompanied by language problems and speech difficulty. With either type of blockage, the microemboli dissolve within hours and full function returns.
Diagnosis
The goal of diagnosis is to identify the precise cause of the TIA and to recommend treatment. Initial information that an individual can supply includes a medical his- tory, what drugs are currently being taken and why, and a full description of the symptoms. Blood tests are ordered to screen blood counts—that is, the numbers of specific blood cell types—and to measure sugar and lipid (fats, including cholesterol) levels. Based on this information and a physical examination that includes blood pressure, pulse, and respiration measurements, one or more of the following imaging tests are ordered.
A computed tomography scan (CT scan) or a magnetic resonance imaging (MRI) scan is usually the first imaging test. CT or MRI can rule out other problems, such as a tumor or subdural hematoma, which can mimic the symptoms of a TIA. A CT scan can also uncover aneurysms and arteriovenous malformation, both of which are blood vessel abnormalities that can cause bleeding in the brain.
Another imaging test that is very useful is carotid ultrasonography, a non-invasive procedure that allows examination of the interior of the carotid artery. This examination can detect carotid stenosis, a condition in which the artery is abnormally narrow because of atheosclerosis. Ultrasonography is very reliable in identifying stenosis, but it does not give enough information to accurately assess the degree of stenosis. Because the treatment used depends on the degree of stenosis, treatment decisions cannot be based on ultrasonography. Another type of ultrasonography, called transcranial doppler ultrasonography, is used to detect stenosis of the blood vessels within the brain and in the vertebrobasilar arteries.
If stenosis is identified, a further test called cerebral arteriography may be done. This test is not done if the individual is in poor health, because it may be too risky. Arteriography involves injecting a special dye into the blood vessels which makes them visible on x rays. This procedure is also used to find suspected problems with blood vessels in the brain. Because it is an invasive procedure, complications may arise. Typically, these complications are minor and temporary. In a very small percentage of people with cardiovascular disease, the procedure may cause serious complications, such as stroke.
Although TIAs affect the brain, the ultimate cause of the problem may be found in the heart. Heart disease or damage to the heart’s blood vessels is assessed by echocardiography. Echocardiography is a type of ultrasonography and is a non-invasive procedure.
Treatment
Treatment is aimed at preventing further TIAs and especially at preventing a stroke. The particular therapy depends on the root cause of the TIA and is not begun until this cause is identified. If at all possible, drug therapy is the preferred method of treating TIAs. Surgical intervention may be required if an individual’s situation is not likely to respond to medication or if medication has failed.
Aspirin is often chosen for drug therapy. It is some- times called a blood thinner because it blocks the function of platelets, the sticky cells that trigger blood clot- ting. Since aspirin can cause gastrointestinal side effects, other drugs may be prescribed. These drugs include dipyridamole or ticlopidine hydrochloride. Dipyridamole, which works by relaxing the smooth muscles of the arteries, is not as effective as aspirin. Ticlopidine hydrochloride is an anti-platelet drug that is slightly more effective than aspirin, especially in women. How- ever, it may cause diarrhoea or lowered blood cell counts. Blood tests must, therefore, be done frequently when patients are taking ticlopidine.
If carotid arteriography reveals at least a 70% blockage of the carotid artery, surgical treatment is usually recommended. The particular surgical method is called carotid endarterectomy. In endarterectomy, the artery is opened and the material clogging it is removed. Another procedure, called angioplasty, has been suggested for treating carotid stenosis, but it is not widely used. This procedure is performed by threading a thin tube through the blood vessel to the site that is clogged. A balloon or a stent (a slender rod) is then passed through the tube to mechanically widen the narrowed area. This procedure is successfully used in other blood vessels in the body, but there is some worry that using it close to the brain may be too dangerous. Surgical treatment of blockage of the vertebrobasilar arteries is not usually recommended.
Treatment of TIAs also focuses on underlying problems. High blood pressure, heart disease, and high levels of blood lipids all require medical intervention. Condition-specific medications are often prescribed and lifestyle changes are strongly encouraged. These changes include giving up smoking or excess alcohol consumption, engaging in physical exercise, and eating sensibly.
Prognosis
One-third of TIAs are followed by stroke in next five years; in the other two-thirds, the TIAs may either continue or disappear on their own. However, because of the risk of stroke-related disability and death, all TIAs should be treated as emergency medical situations.
Medical treatment significantly decreases the risk of stroke for people who experience one or more TIAs. Anti-platelet therapy with aspirin or ticlopidine may reduce risk as much as 31%. Carotid endarterectomy also substantially reduces stroke risk. The procedure itself carries some risk, but the complication rate is less than 5%. The risk of complication can be lowered by choosing to have the procedure done in a facility experienced with it and by a surgeon with a low complication rate.
Prevention
Treatment for TIAs is complemented by lifestyle changes. These practices may also prevent TIAs and strokes from ever occurring. Doctors and other healthcare providers universally recommend that individuals stop smoking and consume alcohol in moderation. Regular health check-ups can detect high blood pressure, heart disease, and other underlying problems. Adhering to treatment for these problems can help minimize TIA and stroke risks. Finally, maintaining a healthy weight and engaging in regular exercise as able are strongly recommended.
(Author is registered medical doctor and health columnist. Feedback: [email protected])