TAKING RESPONSIBILITY
The Role of Surgical Checklists in Ensuring Safe Surgical Practices
In recent years, the healthcare industry has been shaken by alarming reports of wrong-site surgeries, where procedures are performed on the incorrect part of the body or even on the wrong patient. One such incident that went viral recently on social media involved a private hospital where a patient’s uterus was mistakenly removed instead of the scheduled head and neck surgery leading to closure of OT after public outcry. This shocking error raises critical questions: Why do such mistakes occur, and why aren’t there robust systems in place to prevent them? The answer lies in the implementation of standardized safety protocols, such as the World Health Organization (WHO) Surgical Safety Checklist introduced in 2008, and same modified form I introduced in 2012 at SKIMS when I was invited for lecture on,” Safe Surgery practices,” form which has been proven to significantly reduce surgical errors. Who bothers in J&K to improve system? This article explores the causes of wrong-site surgeries, the effectiveness of surgical checklists, and the urgent need for their widespread adoption in healthcare systems worldwide.
The Problem of Wrong-Site Surgeries
Wrong-site surgeries are considered “never events”—errors that should never occur in healthcare. Yet, they continue to happen, often with devastating consequences for patients and their families. These errors can include operating on the wrong side of the body, performing the wrong procedure, or even operating on the wrong patient. The causes of such mistakes are multifaceted and often stem from systemic failures, including miscommunication, lack of standardized protocols, time pressures, and human error. In the case of the viral incident, the removal of a uterus instead of performing head and neck surgery highlights a catastrophic breakdown in communication and verification processes. Such errors are not only tragic but also entirely preventable. The question then arises: Why aren’t healthcare systems doing more to eliminate these preventable mistakes?
The WHO Surgical Safety Checklist: A Proven Solution
In 2008, the WHO introduced the Safe Surgery Checklist as part of its Safe Surgery Saves Lives initiative. This checklist is a simple, yet powerful tool designed to enhance communication and ensure that critical safety steps are followed before, during, and after surgical procedures. The checklist includes a time-out procedure (TOP), which is a final verification step conducted just before the surgery begins. During the TOP, the surgical team reviews the patient’s identity, the planned procedure, and the correct surgical site. This step ensures that everyone on the team is on the same page and that any discrepancies are addressed before the first incision is made.
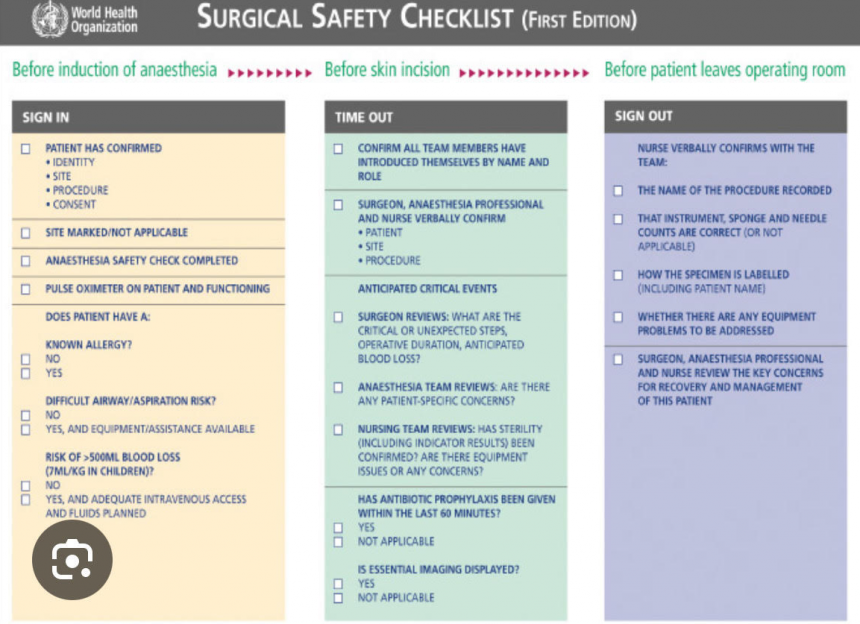
The WHO checklist is divided into three phases:
- Before Induction of Anesthesia (Sign In): Confirms patient identity, procedure, and consent, and checks for allergies or potential complications.
- Before Skin Incision (Time Out): Verifies the correct patient, procedure, and site, and ensures all necessary equipment and imaging are available.
- Before the Patient Leaves the Operating Room (Sign Out): Reviews the procedure, instrument counts, and post-operative care instructions.
How Surgical Checklists Reduce Errors
The use of surgical checklists addresses the root causes of wrong-site surgeries by introducing a standardized process that minimizes the risk of human error. Here’s how:
- Patient Verification: The checklist ensures that the patient’s identity, procedure, and surgical site are confirmed multiple times before the surgery begins. This step alone can prevent errors such as operating on the wrong patient or the wrong side of the body.
- Surgical Site Marking: The checklist requires the surgical site to be clearly marked before the patient enters the operating room. This visual confirmation reduces the likelihood of operating on the wrong site.
- Time-Out Procedure: The TOP is a critical step that brings the entire surgical team together to review and confirm all details before the procedure begins. This pause allows for any last-minute corrections and ensures that everyone is aligned.
- Instrument and Equipment Check: The checklist includes a review of all necessary instruments and equipment, reducing the risk of complications due to missing or malfunctioning tools.
- Post-Procedure Review: The final phase of the checklist ensures that all documentation is accurate and that the patient receives appropriate post-operative care instructions.
Evidence of Effectiveness
Numerous studies have demonstrated the effectiveness of surgical checklists in reducing errors and improving patient outcomes. For example, a landmark study published in The New England Journal of Medicine found that the use of the WHO Surgical Safety Checklist led to a 30-50% reduction in surgical complications and mortality rates. Similarly, the Joint Commission’s Universal Protocol emphasizes the importance of checklists in preventing wrong-site, wrong-procedure, and wrong-patient surgeries. Despite this overwhelming evidence, the adoption of surgical checklists has been inconsistent across our JK healthcare systems. Some hospitals have fully embraced the checklist, while others have been slow to implement it or have failed to use it consistently. This inconsistency highlights the need for stronger leadership and accountability in ensuring the widespread adoption of these life-saving tools.
Barriers to Implementation
While the benefits of surgical checklists are clear, several barriers hinder their implementation:
- Resistance to Change: Healthcare professionals may resist adopting new protocols due to skepticism, lack of training, or the perception that checklists are time-consuming.
- Lack of Leadership: Successful implementation requires strong leadership and a culture of safety. Without buy-in from hospital administrators and surgical teams, checklists are unlikely to be used effectively.
- Inconsistent Use: Even when checklists are introduced, they may not be used consistently. This inconsistency undermines their effectiveness and leaves room for errors to occur.
- Resource Constraints: Some hospitals, particularly in low-resource settings, may lack the infrastructure or personnel needed to implement and monitor checklist use. This form uses A4 one page -what resource constraint.
The Call to Action: Who Will Take Responsibility?
The question remains: Who will take the lead in ensuring that surgical checklists are implemented and used consistently across healthcare systems? The responsibility lies with multiple stakeholders, including:
- Healthcare Administrators: Hospital leaders must prioritize patient safety by mandating the use of surgical checklists and providing the necessary resources and training.
- Surgeons and Surgical Teams: Healthcare professionals must embrace the checklist as a critical tool for ensuring patient safety and use it consistently in every procedure.
- Policymakers: Governments and regulatory bodies should establish guidelines and standards that require the use of surgical checklists in all healthcare facilities.
- Patients and the Public: Patients can advocate for their own safety by asking their healthcare providers about the use of checklists and other safety protocols.
Preventing Disasters Before They Happen
The tragic case of the wrong-site surgery that went viral on social media serves as a stark reminder of the consequences of failing to implement proven safety measures. The WHO Surgical Safety Checklist is a simple, cost-effective tool that has been shown to significantly reduce surgical errors and improve patient outcomes. However, its effectiveness depends on consistent and widespread adoption. We don’t need to wait for disasters to happen before taking action. The time to act is now.
By embracing surgical checklists and fostering a culture of safety, healthcare systems can prevent wrong-site surgeries and ensure that every patient receives the safe, high-quality care they deserve. The question is not whether we can afford to implement these measures, but whether we can afford not to. The answer is clear: Wrong-site surgeries are preventable errors, and it is our collective responsibility to eliminate them.
(The author is a surgeon at Mubarak hospital, Certified and qualified International expert on Healthcare standards of Quality and safety and can be reached at: [email protected])